Queens Medical Professional
Association (QMPA)
Abstract
Queens Medical Professional Association is seeking a grant to fund our
new CARE Program. The program aims to increase integration of Electronic
Health Records (EHR) into the primary care medical practices in order to roll
out an experimental new payment model. The new flexible payment models in
turn are expected to increase health care access in the medically underserved
areas of Queens. QMPA’s first objective is to implement a new payment model
by the end of the first year after studying the intricate details of each
practice and developing new well-tuned workflows. The second year will be
focused on the evaluation of 10 core assessments to aid in determining the
success of the program. QMPA request for $834,249 in order to form the new
program and train other medical professionals from the primary care sites
throughout Queens.
Table of Contents
Statement of Need 3
1.1 QMPA Core Assessment Review Evaluation Project 3
1.2 The Alternative Payment Models and Value Based Payment 7
Year 1: Understanding the Organization of Private Practices 12
Year 2: New Payment Models and Evaluation Changes 17
Organizational Capacity 18
2.1 Organization and Administration 18
Finance Branch 19
Healthcare Section 20
Social Provisions Division 20
2.2 Operational Plan 20
2.3 Organization Structure and Staffing 21
Funding and Sustainability 22
3.1 Budget Narrative 22
3.2 Model Sustainability 25
Evaluation 25
Supporting Documents 27
Appendix 1 – Placement of the CARE Program within QMPA 27
Appendix 2 – CARE Program 27
Appendix 3 – Overall Total Project Budget for Electronic
Healthcare Initiative 28
Statement of Need
1.1 QMPA Core Assessment Review Evaluation Project
The Queens Medical Professional
Association plans to initiate its CARE program with three main objectives:
1. Clinical
Care Team Transformation
2. Clinical
Electronic Integration
3. Financial
Planning, Implementation, and Control
Clinical care team transformations
will require a push by healthcare professionals to learn the ins and outs of
the software. To aid them are our frontline project managers and technology
specialists. After the initial observation of each medical practice, the main
office of the organization will host a weekly workshop to address ongoing EHR
issues and possible improvements from suggestions surveyed. Project managers
will have to actively take part in the learning process to make sure that the
healthcare professionals do not feel overburdened by the process.
Clinical electronic integration is
the crux of heavily integrating practices with new electronic health records
(EHRs). Integration means that the EHRs are utilized at a greater level than
just a record-keeping device. It means that the records are actively being
used during collaboration with other healthcare professionals for wide
reaching projects and quality improvement measures. Other aspects of EHRs are
to enable the health care provider to gain access to the patient’s full
medical history through hospital, group practice and private company data.
Financial planning,
implementation, and control will be the main emphasis for the second phase of
the program when it switches from quality measures and EHR improvements to
payment model adaptation. Their needs to be a strict accounting system in
place to calculate the potential revenue, loss money from denied claims, cash
flow from cost sharing measures (such as copay and coinsurance), and other
possible expenses. The new model must be shown not only as making more
revenue, but also being efficient. An increase in revenue will mean little if
the staff is constantly working overtime. Gains in revenue can be reallocated
towards improving patient quality of care.
Technology, while infinite in its
potential, continues to struggle in its adaption to various human complex
adaptive systems. In 2009, Health Information Technology for Economic and
Clinical Health (HITECH) Act earmarked nearly $30 billion towards electronic
health record adoption and meaningful use (Rosenbaum, 2015). However, despite
massive government incentive towards the implementation of electronic health
records, hospitals and private practices have struggled to fully integrate
technology into the healthcare setting. The year 2012 brought a substantial
increase in EHR participation in both the hospital and professional practice
setting with 63.8% of eligible hospitals participating and 48.0% of eligible
professionals participating (US Government Accountability Office, 2014). Since
then there has been a trend of increasing physician participation in
electronic health records. Unfortunately, despite the increased participation,
many of the EHRs have been used for syndrome surveillance, laboratory
reporting, and registries instead of public health efforts (Friedman, Parrish
& Ross, 2013).
Another issue, is closely tied to
EHRs is reimbursement. The traditional payment model was the fee-for-service
reimbursement where cost of treatment was tied to type of service provided.
Unfortunately, this payment model incentivizes medical professionals to
overprovide healthcare services (Porter, 2012). Valued based reimbursement
instead attempts to focus on patient metrics to determine reimbursement. This
is not the only alternative reimbursement plan available. Other alternatives
that have been tested are capitation payments and bundle payments. Capitation
payments are regular lump sum payments given to the provider regardless of
number of services utilized. The
integration of EHRs enables the tracking of metrics, which makes value based
reimbursement possible.
The combination of healthcare and
technology contains massive untapped potential. The ability to coordinate
public health programs with physicians dispersed throughout a region on
massive scale with immediate adequate health feedback opens the field to
tele-health. Not only would the public health officials be able to perform
epidemiology on a massive scale, but patients would also be able to access
their health records when needed. In addition, the interconnection of the
health records with major medical institutions would enable treatments with
thorough patient history provided by the primary care provider. However,
implementation hiccups have stalled these visions of technology integration. The
Queens Medical Professional Association aims to aid medical providers in
gradually implementing changes over time to create a smooth transition towards
efficient EHR integration into the private practice workflow. The purpose of
the project is to lay the groundwork for possible later implementations of a
new payment model.
Queens Medical Professionals
Association (QMPA) intends to confront the fee-for-service model still present
in the primary care practices of Queens to improve healthcare access and
streamline primary care practices. According the US Government census, the
borough of Queens in New York City has a population of 2,333,054 residents.
Within this group reside some 5,049 physicians. Of the total number of
physicians, 1,897 are primary care providers (Robert Graham Center, 2015).[1]
Queens has lower physician to population ratio than New York State overall
with certain areas such as Corona, Jamaica, and Astoria designated as
medically underserved areas. This ratio indicates the strain placed on the
present primary care physicians attempting to maintain the health of their
respective neighborhoods. What medical care is available is often swamped with
numerous patients. Doctors within the neighborhood of Flushing and Elmhurst
have reached patient loads of over 2,000 per primary care provider.[2]
Doctors are not required to accept large patients loads, however, they do so
in order to maintain their revenue stream as insurers have paid less for
“nonessential” services. Predictably, the large patient loads result in
shorter face-to-face interactions with the doctor ranging from a maximum of
one hour to a minimum of 15 minutes. A doctor with an average of 30 patients
daily would require at least 15 hours to provide quality healthcare, difficult
to achieve even in the best of conditions.[3]
Heavy time burdens as well as lack of incentives discourage physicians from
coordinating patient care with other healthcare professionals. The end result
is an endless array of paperwork back and forth with other health
institutions, over issues patient issues that may have been already covered a
month ago.
QMPA’s efforts will be directed
towards the neighborhood of Corona. Corona presents a perfect preliminary
testing ground for a transition to value-based healthcare. Like most of
America, its population suffers from rising chronic health issues such as a
25% obesity rate and a 14% diabetes rate. 66% of the population is foreign born
and 53% of neighborhood has limited English proficiency (NYC DOHMH, 2015). The
cultures from this neighborhood vary widely and will significantly affect
patient relations with medical professionals. Overcoming these challenges will
demonstrate that the program is scalable to the rest of Queens.
While there have been government
incentive programs towards the implementation of EHR systems at private
practices such as HITECH, they often lack detailed instruction on how to
effectively use EHRs within the medical workflow. Other programs such as PCMH
focus only on the specific on aspects of the EHR such as registry reports.
Building on the past experiences of IT specialists, group health insurance,
value reimbursement programs, and government efforts, this programs seeks to
solidify the connection between EHR and primary care.
1.2 The Alternative Payment Models and Value Based
Payment
A total of 30 clinics have agreed
to participate in the CARE program. They are scattered throughout the Queens
area stretching from Astoria to Jamaica. While project is mainly focused on
the neighborhood of Corona with its 10 medical clinics, other practices
throughout Queens are also involved to see if the program is flexible in
different environments.
At the center of the program are
ten core assessments of quality healthcare:
1. Cholesterol
management
2. Cancer
management
3. Hypertension
treatment
4. Diabetes
management
5. Obesity
management
6. Mental
health Guidance
7. Gastro-intestinal
health (report on bowel movements, treatment plans)
8. Smoking
(treatment for addiction, long term plan)
9. Drinking
(report for liver function, treatment for addiction, long term plan)
10. Healthcare
cooperation (P2P referrals, online portals, shared patient access)
These ten objectives are to be
promoted at 30 primary care practices and are the core focus of the basic
reports.
Cholesterol management
concentrates on the results of lipid panel blood tests. The usual range of
cholesterol is less than 200mg/dL (Laberge, 2013). Often patients with an
overconsumption of fat in diet, a lack of exercise, or a genetic disorder
suffers from hyperlipidemia and other related cholesterol diseases. The levels
of cholesterol are generally asymptomatic in that they do not directly cause
diseases. Rather they serve as cofactors to other issues such as emboli and
thrombi development. The favored medications for treatment of
hypercholesterolemia (aka hyperlipidemia) are statins. Monitoring the total
cholesterol levels and medication schedule will enable for the development of
future long-term plans.
Cancer management is focused on
detecting the cancers when they are in the early stages of 0 and I. Early
treatment prevents the cancer from metastasizing and developing into stages II
– IV. The management of cancer will be difficult considering that there are so
many different types of cancers possible for various organs throughout the
body. A pap smear is used to determine cervical cancer. A mammogram is used to
determine breast cancer. CBC blood tests can be used to determine cancer of
different types of blood cells. What will be vital to the process is recording
the initial diagnosis/discovery and connecting it to the prognosis and overall
outcome. Steps must be taken to connect the electronic health records of the
primary care and of the oncologist. This integration will help for better
treatment or prevention of cancer relapse.
The medical community recently has
switched to new hypertension guidelines following the 140/90 to
130/80-baseline change. These new guidelines are expected to help in
preventative healthcare as treatment of hypertension early will help prevent
the rise of later chronic correlated diseases. However, even the experts are
still debating about the controversial guideline changes (Bakris, 2018). Some
common medications used for treatment of hypertension are diuretics,
beta-blockers, and ACE inhibitors. Analyzing the progress of medication
overtime will help determine if treatment is effective.
Diabetes measures will be based
off HbA1c levels as well as current glucose levels. The HbA1c test will be
used to determine whether or not the patient has diabetes, pre-diabetes, or no
diabetes. Treatment will also vary depending on the severity of the disease. Depending
on the medical practitioner’s decision, patients will be given a specific type
of medication such as metformin. The medication consumption and overall
schedule will be recorded on the EHR. For patients already with the diagnosis
of diabetes, the glucose levels will be monitored through the finger prick
tests. Glucose levels over time will be observed through integrated blood
testing machines.
Obesity diagnosis are closely
linked to the patient’s body mass index (BMI). The acceptable BMI range varies
depending on the gender and age. For adults the commonly held parameters are
that a BMI under 18.5 is considered underweight while a BMI of 30 or more is
considered obese (McPherson, 2008). For children and adolescents BMI
percentiles are used for an overall comparison with the rest of the
population. The gathering of BMI data will be simple considering the
collection of weight and height during almost every physician office visit. The
important factor will be to look out for possible comorbidity with other
diseases such as diabetes or coronary artery disease.
Mental health has long puzzled
primary health care practitioners. Often little resources or follow up are
provided by primary care physicians. Most mentally ill patients are referred
to a psychiatrist or other mental health services with little to no integration
between the services. The stigma of mental illness persists to this day,
however, primary care practices have a duty to perform a first level of care. One
of the most common mental illnesses is depression. Physicians should look
carefully into the patient’s behavior for possible signs of depression and
complete the assessment with PH-2 and PH-9 questionnaires. There is a strong
emphasis on collaborating with other mental health services to make sure that
the patient is attended to early to prevent exacerbating the situation later
on.
Digestive tract health is of
especial vital importance for the elderly and those with other comorbid gastrointestinal
diseases. Poor bowel movements, difficulty excreting stool, and bowel
incontinence heavily affect one’s quality of life and can exacerbate other
health conditions. For this reason close integration with the gastrointestinal
specialist is needed to make sure patients received a full consultation and if
needed, an endoscopy.
Smoking and drinking are
considered lifestyle decisions that can negatively impact your health. The
correlation between smoking and lung disease is strong, but not guaranteed.
The same issue can be seen with the consumption of alcoholic beverages and its
connection to liver disease. For the primary care physician, these guilty
pleasures will be difficult to wean patients off of. The primary determination
needed before starting smoking cessation and or alcohol counseling will be the
patient’s decision. If and only if the patient fully participates in the
program will full resources be utilized.
Healthcare cooperation is a factor
that will be based off multiple different measures. One of the easiest ways to
measure healthcare integration is to record the sharing of patient charts and
the utilization of e-referrals. Other more difficult aspects are the meetings
between healthcare workers regarding a specific patient’s needs. These will
have to be recorded through fax, email, or logging if done through telecoms.
The program is broken into two
parts:
1. Year
1: Understanding the Organization of Private Practices
2. Year
2: Evaluation Changes and New Payment Models
Year 1: Understanding the Organization of Private
Practices
While the general structure of a
primary care office remains unchanged, each practice has its own work
organization and workflow. A specific study must be undertaken to determine
the weaknesses and the strengths of each practice. Within the first month a
project manager should have visited and observed their 10 assigned medical
practices at least three times. Each project manager should have acquired the
5 W’s of each practice. Who are the employees (details on the staff)? What are
the procedures and policies of the practice? Where is the practice established
and from where does majority of its patients hail from? When is the practice
open? How does the practice’s policies and time organization affect the overall
practice and its interaction with patients? Besides these basic five points,
the project managers are free to choose what they considered vital to the
report.
On the last day of the first month
of the initiative, the program managers will submit a preliminary report on
the status and condition of their 10 assigned medical practices. Then, a
meeting will be held involving all members of the project to discuss potential
hazards for each clinic. Focus will be placed on the top three expected
difficult medical practices with the ultimate goal of working out any kinks
before implementation of continuous quality improvement (CQI).
A tally will also be made to determine which
are the five top EHRs among the 30 medical practices. The EHR specialist and
IT assistant will focus their efforts on the EHR priority list. However, the
IT assistant will focus more on the well known EHRs that have more product
support, while the EHR specialists centers their attention on the more obscure
EHRs.
On the second month, the project
manager will write a similar basic report with greater emphasis on small
nuances of each employee at the practice. However, this time the project
manager will extract patient data from the practice’s EHR to determine out of
the entire patient population, which patients require follow up services or
treatment for the core measures listed above. Separate lists of patients will
be generated for each core assessment.[4] Once
the list for each core assessment is complete, the project manager will
compile a separate report with the data. The report will describe the
practices’ overall first stage of patient treatment percentage and follow up
treatment percentage on each of the core assessments. A review of the report
will allow us to determine, which of the ten sectors the physician is lacking
in. Project managers can identify areas needing improvement and can focus
their efforts on cooperating with practices to increase patient data
transparency.
Core assessment number 10 will use a different formula for
the report.
The expected score of a first time
pass without any changes in policy will be a lenient cut off of 50%. The
expectation is that the score will rise overtime as some improvements have
been made.
The results of the report must be
discussed with physicians, allied health staff, and administrative workers to
determine if there is an error with EHR data compilation. Sometimes healthcare
practices forget an extra click or neglect to use structured data resulting in
skewed results when using the registry. A randomized 10% of patient records
from each practice will be pulled from the patient groups with one of the nine
health-related conditions as well as 10% from the patient group without the
conditions. The randomly selected groups will be analyzed for health history
and to determine if the necessary conditions exist or that the patient’s
health falls into the parameters of listed health condition. Only after this
preliminary check is completed can suggestions of changes can be done.
With both reports in hand, the
project managers will have another meeting, this time with the president and
executive assistant. The group will go over the possible suggestions and improvements.
Suggestions for improvements have three tiers:
Low tier suggestions are EHR
methodology changes. QMPA provides EHR training for reporting and data
management as well as consultation regarding system integration of new payment
models. Often physicians and associated medical staff are not familiar with
the updates and expanded capabilities of their EHR software. All too often
only the base requirements of the program such as appointment scheduling and
SOAP note writing are utilized. Project managers up to date on the latest EHR
software will be able to point out how new chains of commands can streamline a
billing process or how template usage can be adapted for patients.
Middle tier suggestions are to
allied health or physicians. Perhaps the physician has been using one test as
a core part of his assessment when there would be other more effective tests.
Or perhaps allied health staff was unaware of recent research findings on a
specific procedure. Recent research findings can be integrated into practices’
for a more efficient method of introducing treatment change.
Top tier suggestions are
policy-based changes that will dramatically affect the practice’s workflow and
patient interactions. Hiring auxiliary staff to handle insurance and other
medical paperwork in conjunction with using other health practitioners is a
few of such examples. The considerable change to the structure of the practice
will require group huddles and concentrated dedication to the new model system
developed.
On the third month, project
managers will implement the suggestions and turn theory into practice. Working
with medical professionals, project managers will coordinate the various
suggestions worked out at the meeting. At the same time, QMPA will start to
host weekly workshops regarding EHRs as well as meetings for improved workflow
designs. The weekly workshops will be held on a weekday or weekend depending
on medical professional availability. Each workshop will feature three EHR
software programs and their order sequences for analyzing core health
assessments. Also will include specific troubleshooting questions and possible
efficiency improvements. Finalized workflow charts of each practice are
devised after the project manager believes he or she has sufficient
understanding of the practice’s ins and outs. Evaluation of the suggestions
occurs after three months or a quarterly. After a cycle of suggestion/improvements
and evaluations, the end of the first year will bring the significant top tier
improvement, a new payment model.
Year 2: New Payment Models and Evaluation Changes
Research from the prior year is
used to determine the suitable alternate payment options to offer to different
medical practices. For practices looking to maintain independent from hospital
affiliations and group practice networks, retainer-based practice, with its
direct payment model from patient to physician. For practices with a large
share of Medicaid and Medicare patient, shared savings programs would be more
suited. For practices that see patients with insurance from large employers
such as government agencies, Accountable Care Organizations might be the way
to go. Regardless, most these major changes to the payment model are not
expected to result in major financial hardship for practices (Friedberg, Chen,
White, Jung, Raaen, Hirshman, & Lipinski (2015). The start of the New Year
will be an optimal time to introduce a new payment model, as both the medical
professionals and the patient will have their spirits buoyed by the
festivities. The next four quarterlies will be centered on evaluations of the
new payment model and the continuing quality of the 10 core assessments.
Changing payment models is
expected to cause a considerable amount of confusion for older primary care
physicians with less developed systems. Greater effort in terms of
consultation and training will be provided to these practices. Another issue
bound to turn up is the lack of patient healthcare progress. Unless there is
significant social, economic incentive and or willpower, many patients will
struggle to break old habits and routines. For these issues, referrals to
specialists, counselors and or patient management companies are recommended.
The third problem is that Electronic Health Records(EHR) software is not
standardize and the different software will make coordinating efforts
difficult. Our trainers will take a survey of EHRs being used by the 30
primary care providers. After compiling a list of EHRs, our trainers will
contact the EHR companies for software demonstrations.
Organizational Capacity
2.1 Organization and Administration
Queens Medical Professional
Association has a ten-year history of aiding medical professionals. It all
started ten years ago on December 2008 with the US markets collapsing under
the weight of the subprime mortgage crisis. Doctor Omnes Amigon and his group
of medical friends came together to discuss the inevitable increase in
patients without insurance. In addition, with the new president’s pledge to
reform healthcare there was a storm brewing for healthcare industry that was
bound to upset the current standard. With their practices in Astoria, Jackson
Heights, and Corona, the doctors decided that they needed to band together to
provide health services to the community in this time of great need. At the
same time, this new group of medical professionals would provide a vital networking
tool to discuss daily issues encountered at their practices and ways to
improve them. They formed the Queens Medical Professional Association with the
first goal of setting up a community health fair.
The first community health fair
was held on August 2019 at the Dutch Kills Playground in Astoria with
cooperation from the Department of Health and Mental Hygiene, Department of
Parks and Recreation, and local church groups. Since then, the organization
has held the annual community health fair at different parks throughout
Astoria, Jackson Heights, Corona, Elmhurst, and Woodside. At the health fair
doctors provide blood pressure readings, glucose readings, basic vitals check,
and health consultations. Each participant in the health fair was provided a basic
health folder packed with preventative health education and their subjective,
objective, assessment, plan (SOAP) note of the day. At the end before leaving
the health fair, a volunteer takes the carbon copy of the patient’s SOAP note
and keeps it on file. During the next weekend, the doctors will pick out
particular worrying cases to follow up on.
Collaborations with community
organizations were vital to our organization’s initial success in providing
care to many patients. About 36% of the population of Corona and Elmhurst do
not have any form of health insurance (King, Hinterland, Dragan, Driver,
Harris, Gwynn, & Bassett, 2015). Thus, it was more likely for these
individuals during crises of health to go to the local hospital or community health
centers.
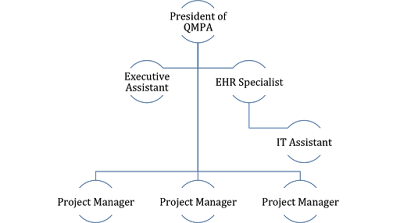
The structure of QMPA is based on
the hierarchical model of organization. The founder, Doctor Amigon, is the
association’s president. Under him are three basic sections of the
organization: Finance Branch, Healthcare Section, and Social Provision
Division.[5] The
newly proposed CARE program would be placed under the healthcare section.
Finance Branch
John Chen CPA, has run the finance
department since its original creation in 2008. He is a close friend of Dr.
Amigon and aids in sorting out the association’s finances. Helping him is our
resident, retired bookkeeper, Sally Hu. Sally was originally a patient of Mr.
Amigon and leapt and the chance to participate in community affairs.
Throughout the years they have been aided by accounting interns brought over
from the CUNY Colleges. Both, Sally and John have done a fantastic job at
organizing the money pooled at events for future events. They have also help
the organization keep track of expenses and provided reports for expected
future expenses.
Healthcare Section
The health section is blessed with
Dr. Amigon’s close friends from medical school. It comprises of a group of 12
doctors all in primary care. Over time the group has expanded to include
specialists and other allied health professionals such as medical assistants.
Social Provisions Division
The social section is composed of
church and other religious leaders as well as nongovernment organizations from
the neighborhoods. Old friends Sammy Lopez and Daisy Lopez, restaurant
storeowners from Corona, lead the social section in community discussions at
parks, hospices, church, bingo halls, and town hall meetings. Both have just
recently retired from the food industry and have poured their soul into
community efforts.
2.2 Operational Plan
Out CARE program will be working
alongside religious organizations from the Eternal Love Baptist Church, NY
Dong Yang First Church, St. Paul The Apostle Church, Queens Church of Christ,
and the Latin American Pentecostal Church. The first and second year
objectives also coincide with NYC government community health efforts within
the neighborhood.
2.3 Organization Structure and Staffing
For our program we have formed a
specific team of seven people for the task.[6]
At the top is President Amigon who directs the general basis of the program.
He oversees the organization’s funding and human networking connections. He is
aided by an executive assistant to deal with a variety of matters ranging from
phone calls to presentation setups. An IT subgroup of two people: EHR
specialist and IT Assistant are in charge of computer related issues. The EHR
specialists will be acquainted with popular EHR software such as Epic, MDLand, eClinicalworks and
allscripts. By being familiar with
the programs, the EHR specialist should also know the possible ways to change
the programming chain. This changing point is where the IT assistant comes in.
The IT assistant will provide computer troubleshooting for the transition
process and during computer system updates. The core of the initiative lies
with the three project managers who will oversee the entire process from start
to finish at the 30 medical practices. They will travel for face-to-face
interactions with the doctors they are assigned to.
Table 1: Roles and Responsibilities
of CARE Program
|
Role
|
Responsibilities
|
|
President
|
Directing program, networking with other execs, General
guidance
|
|
Executive Assistant
|
Administrative tasks: Answering phone, setting
appointments, organizing files in numerical order, writing up meeting
minutes
|
|
EHR Specialist
|
EHR functionality, Software adaption, troubleshooting
|
|
IT Assistant
|
Software clearance, troubleshooting
|
|
Project Manager
|
Physical travel to practices, assessment of practices,
reports, communication skills
|
Funding and Sustainability
3.1 Budget Narrative
QMPA has estimated the cost of the
two-year value based health care program to be $834,240. This cost is gathered
from annual salary, fringe benefits and organizational expenses and
multiplying that total, $417,120 by two to get $834,240. A further breakdown
of the individual portions of the total annual cost is available below.
|
Type
of Expense
|
Cost
|
|
Personnel
|
$375,204.00
|
|
Other Than Personnel Expense
|
$41,916.00
|
|
$417,120.00
|
|
|
Two year cost expense
|
$834,240.00
|
Table 2: Annual
QMPA Expenses
The president’s salary is not
included on this list as the organization already provides him with
significant perks and benefits. The executive assistant is given $37,440. The
EHR specialist is given $54,600 for their technical computer software
expertise. Their skills and knowledge will be actively applied to maintain the
program schedule. The IT assistant has a low salary of $31,200. The hope is to
hire a student graduate of computer science searching for experience for later
career advancement. Each project manager has a salary of $49,400 each for a
total of $148,200 for the three of them. Since they will perform the brunt of
the on the ground activities, they will be granted the most leeway in terms of
flexible time schedules. Additional project managers may be sought if the
patient care workload and time constraints prove to be too taxing.
|
Title
|
#
|
Hourly
|
Hours
|
FTE
|
Weekly Salary
|
Annual Salary
|
Annual Cost
|
|
President
|
1
|
$-
|
-
|
0.00
|
$-
|
$-
|
$-
|
|
Administrative
Assistant
|
1
|
$18.00
|
40.00
|
1.00
|
$720.00
|
$37,440.00
|
$37,440.00
|
|
EHR
Specialist
|
1
|
$21.00
|
50.00
|
1.25
|
$1,050.00
|
$54,600.00
|
$54,600.00
|
|
IT
Assistant
|
1
|
$15.00
|
40.00
|
1.00
|
$600.00
|
$31,200.00
|
$31,200.00
|
|
Project
Manager
|
3
|
$19.00
|
50.00
|
1.25
|
$950.00
|
$49,400.00
|
$148,200.00
|
|
|
7
|
$73.00
|
180.00
|
|
$3,320.00
|
$172,640.00
|
$271,440.00
|
Table 3: Salary
Breakdown of Staff
Fringe benefits include a health
savings account, a free monthly metro card, and childcare that are 38% of the
original salary provided. The health savings account will be a portion of a
group health insurance program with a total annual cost of $42,000. Health
expenses from medication to copay will be considered a valid expenditure of an
employee’s health benefits. For transportation, each staff member receives a
monthly-unlimited MTA metro card at the price of $121 per person for a total
of $10,164. Substantial traffic as well as difficulties with parking has lead
to the use of the metro card instead of a shared organization car. A childcare
fund of $1,000 monthly is available for those with children under 21. The
childcare fund can be used for anything child related from babysitting to
healthy food. Both the health savings account and the childcare fund roll over
and do not expire.
|
Type
of Benefit
|
#
|
Monthly/Person
|
Annual Cost/Person
|
Cost to Organization
|
% Salary Cost
|
|
Health
Savings Account
|
7
|
$400.00
|
$4,800.00
|
$33,600.00
|
12.38%
|
|
Child
Care
|
5
|
$1,000.00
|
$12,000.00
|
$60,000.00
|
22.10%
|
|
Transportation
|
7
|
$121.00
|
$1,452.00
|
$10,164.00
|
3.74%
|
|
19
|
$1,521.00
|
$18,252.00
|
$103,764.00
|
38.23%
|
Table 4: Fringe
Benefits
The rent for the association’s
headquarters is provided at discount cost. The utilities, including water,
electricity, phone, and heat, are compounded together, also at discount cost,
for $60 a month. The meeting fees and travel expenses are allocated to long
distance travel to conferences and meetings with other professionals involved
with healthcare technology and organization. Training expenses will fund the
weekly workshops held at the association, while the consultation costs will be
contractual depending on the stage of the program. Insurance costs are geared
towards coverage of the activities held by the association. Food costs will be
geared towards catering during workshops and to feed staff. Lunch is covered,
but dinner is not.
|
Expense
|
Monthly
|
Annual Cost
|
|
Rent
|
800.00
|
9,600.00
|
|
Utilities
|
60.00
|
720.00
|
|
Food
|
300.00
|
3,600.00
|
|
Meeting
Fees
|
83.00
|
996.00
|
|
Insurance
Coverage
|
83.00
|
996.00
|
|
Travel
|
83.00
|
996.00
|
|
Structure
& Payment Consult
|
84.00
|
1,008.00
|
|
Training
Class
|
2,000.00
|
24,000.00
|
|
3,493.00
|
41,916.00
|
Table 5:
Organizational Expenses
Thank to donations provided by our
participating providers as well as our individual community members we have
already been provided a significant amount of our office supplies.
Supplementing the office supplies are the food and drinks provided courtesy of
our local convenience stores. These in kind donations provide a savings cost
of $17,960.
|
Type
of Donation
|
Quantity
|
Cost Per
|
Total
|
|
Laptop
Computers
|
10
|
$1,500.00
|
$15,000.00
|
|
Toner
Ink (Boxes)
|
10
|
$100.00
|
$1,000.00
|
|
Printer
All in One
|
1
|
$300.00
|
$300.00
|
|
Writing
Utensils
|
30
|
$10.00
|
$300.00
|
|
Clips,
Staples, Holders
|
30
|
$7.00
|
$210.00
|
|
Filing
cabinet
|
4
|
$50.00
|
$200.00
|
|
Paper
(5000sheets)
|
3
|
$60.00
|
$180.00
|
|
Tables
(Portable)
|
5
|
$40.00
|
$200.00
|
|
Chairs
(Portable)
|
20
|
$15.00
|
$300.00
|
|
Food
(Canned Goods)
|
40
|
$3.00
|
$120.00
|
|
Drinks
(24-Packs)
|
5
|
$30.00
|
$150.00
|
|
2,115.00
|
17,960.00
|
Table 6: In kind Donations
3.2 Model Sustainability
The program hopes to achieve
savings by increasing the flexibility of primary care practices through
alternative payment models. The better alternatives allow greater access to
health care. Running parallel to the new payment models are the improved EHR utilization
efforts. Increased efficiency of the health records will allow allied health
staff to better aid the physician. Having the numbers and the documents on
file will also allow consultants and third party services, when permitted, to compile
reports. The table below illustrates the best possible savings that can be
achieved with better training of electronic health records.
|
Type
of Benefit
|
Quantity
|
Money Opp Cost
|
Number of Patients
|
Gross
Savings
|
|
Cost
Performance
|
30
|
$170.00
|
1,500.00
|
$7,650,000.00
|
|
Physician
Coordination
|
30
|
$10.00
|
1,500.00
|
$450,000.00
|
|
Preventative
Health
|
30
|
$50.00
|
1,500.00
|
$2,250,000.00
|
|
$10,350,000.00
|
Table 3: Possible Health Savings
Evaluation
Evaluation of the entire operation
will be broken into chunks of audits and meetings. Each quarter will be
evaluated through its action process. Since the earlier months are spent
setting up the suggestions and systems, focus will be on the reports produced
by the project managers. These reports will be cross-examined with patient
data and health professional accounts of their clinical operations through a
one-on-one discussion with the health professionals. Of the first three
quartiles all the reports must be accurate to set a strong foundation for
later suggestions. The information must be at least 90% accurate to verify for
a solid foundation. The accuracy will be determined by cross checking with
medical professionals from the private practice. If the first three quartiles
do not reach the threshold of 90%, another round of reports will be required
by the next quartile. This second time more emphasis will be placed on that
specific clinic.
Later quarterlies will focus more
on workshop and suggestion implementation. A survey of the workshops will
provide QMPA staff with overall morale of the healthcare professionals from
each practice. It is expected that some of the practices will have health
professionals with little to no motivation to change policies or workflows.
Hope is to have the possible benefits of new EHR procedures dangled in front
of the health professionals to act an incentive to already existing problems.
Suggestions that are implemented should be evaluated on a before versus after
basis. If at least 50% of the suggestions are successfully implemented, then
the later quarterlies can be considered effective.
To evaluate final long-term
outcomes, we will examine the change in the data connected to the nine core
assessments. Changes regarding practice workflow comparison will be made from
past program manager reports to current conditions. If there is a marked
improvement on at least 50% of suggestions, the program will be considered a
success. In addition, the patients will receive a survey at the end of their office
visit to verify if they identified new payment models as responsible for their
visit.
Supporting Documents
Appendix 1 – Placement of the CARE Program within
QMPA
Appendix 2 – CARE Program
Appendix 3 – Overall Total Project Budget for
Electronic Healthcare Initiative
|
RFP, Project Budget (Required)
|
|||
|
Robert
Wood Johnson Foundation
|
Queens
Medical Professional Association
|
||
|
Expenses
|
Total Project Expenses
|
Amount Requested from Funder
|
|
|
Salary and Benefits
|
$375,204.00
|
$375,204.00
|
|
|
Contract Services (consulting, professional, fundraising)
|
$1,008.00
|
$1,008.00
|
|
|
Occupancy (rent, utilities, maintenance)
|
$10,320.00
|
$10,320.00
|
|
|
Training & Professional Development
|
$24,000.00
|
$24,000
|
|
|
Insurance
|
$996.00
|
$-
|
|
|
Travel
|
$996.00
|
$-
|
|
|
Supplies
|
$17,960.00
|
$-
|
|
|
Evaluation
|
$5,000.00
|
$5,000
|
|
|
Conferences, meetings, etc.
|
$996.00
|
$996
|
|
|
TOTAL EXPENSES
|
$536,840
|
$416,528
|
|
|
Revenues
|
Committed
|
Pending
|
|
|
Contributions, Gifts, Grants, & Earned Revenue
|
|
|
|
|
Local Government
|
$-
|
$50,000
|
|
|
State Government
|
$100,000
|
$-
|
|
|
Federal Government
|
$-
|
$-
|
|
|
Individuals
|
$5,000
|
$-
|
|
|
*Corporation-Jones Surgical Instruments
|
$1,000
|
$-
|
|
|
Membership Income
|
$3,000
|
$1,500
|
|
|
Fundraising Events (net)
|
$500
|
$-
|
|
|
Investment Income
|
$10,000
|
$-
|
|
|
In-Kind Support
|
$17,690
|
$-
|
|
|
TOTAL REVENUES
|
$137,190.00
|
$51,500.00
|
|
References
Bakris, G., & Sorrentino, M. (2018). Redefining
hypertension — assessing the new blood-pressure guidelines. N Engl J
Med, 378(6), 497-499. 10.1056/NEJMp1716193 Retrieved from https://doi-org.ez-proxy.brooklyn.cuny.edu/10.1056/NEJMp1716193
Center for Workforce Studies, Erikson, C., Jones, K.,
& Whatley, M. (2015). 2015 state physician workforce data book.().Association
of American Medical Colleges. Retrieved from https://members.aamc.org/eweb/upload/2015StateDataBook%20(revised).pdf
Clough, J. D., Richman, B. D., & Glickman, S. W.
(2015). Outlook for alternative payment models in fee-for-service medicare. Jama, 314(4),
341-342. 10.1001/jama.2015.8047
Fleurant, M., Kell, R., Jenter, C., Volk, L. A.,
Zhang, F., Bates, D. W., & Simon, S. R. (2012). Factors associated
with difficult electronic health record implementation in office practice10.1136/amiajnl-2011-000689
Friedberg, M. W., Chen, P. G., White, C., Jung, O.,
Raaen, L., Hirshman, S., . . . Lipinski, L. (2015). Effects of health care
payment models on physician practice in the united states. Rand Health
Quarterly, 5(1), 8.
Friedman, D. J., Parrish, R. G., & Ross, D. A.
(2013). Electronic health records and US public health: Current realities and
future promise. American Journal of Public Health, 103(9),
1560. 10.2105/AJPH.2013.301220
Helmchen, L. A. (2009). Fee-for-service. In R. M.
Mullner (Ed.), Encyclopedia of health services research (pp.
399-401). Thousand Oaks, CA: SAGE Publications. Retrieved from http://link.galegroup.com.ez-proxy.brooklyn.cuny.edu:2048/apps/doc/CX3208000153/GVRL?u=cuny_broo39667&sid=GVRL&xid=2d45edc8
Hydari, M., Telang, R., & Marella, W. (2015).
Electronic health records and patient safety. Communications of the
ACM, 58(11), 30-32. 10.1145/2822515
Jha, A. K., DesRoches, C. M., Campbell, E. G.,
Donelan, K., Rao, S. R., Ferris, T. G., . . . Blumenthal, D. (2009). Use of electronic
health records in U.S. hospitals. N Engl J Med, 360(16),
1628-1638. 10.1056/NEJMsa0900592 Retrieved from https://doi-org.ez-proxy.brooklyn.cuny.edu/10.1056/NEJMsa0900592
King, L., Hinterland, K., Dragan, L., Driver, C. R.,
Harris, T. G., Gwynn, R. C., . . . Bassett, M. T. (2015). Community
health profiles 2015, queens community district 4: Elmhurst and corona. ().New
York City Department of Health and Mental Hygiene.
Laberge, M. (2013). Hyperlipidemia. In K. Key
(Ed.), The gale encyclopedia of diets: A guide to health and nutrition(2nd
ed. ed., pp. 613-617). Detroit: Gale. Retrieved from http://link.galegroup.com.ez-proxy.brooklyn.cuny.edu:2048/apps/doc/CX2760100169/GVRL?u=cuny_broo39667&sid=GVRL&xid=39d2a214
Larsen, K. N., Kristensen, S. R., & S�gaard, R. (2018).
Autonomy to health care professionals as a vehicle for value-based health care?
results of a quasi-experiment in hospital governance. Social Science
& Medicine; Social Science & Medicine, 196, 37-46.
10.1016/j.socscimed.2017.11.009
McPherson, D. (2008). Body mass index (BMI). In S.
Boslaugh (Ed.), Encyclopedia of epidemiology (pp. 101-103).
Thousand Oaks, CA: SAGE Publications. Retrieved from http://link.galegroup.com.ez-proxy.brooklyn.cuny.edu:2048/apps/doc/CX2660800057/GVRL?u=cuny_broo39667&sid=GVRL&xid=837b8149
Nussbaum, S., Mcclellan, M., & Metlay, G. (2018).
Principles for a framework for alternative payment models. Jama, 319(7),
653. 10.1001/jama.2017.20226
Office of the Professions. (2018). License statistics.
Retrieved from http://www.op.nysed.gov/prof/med/medcounts.htm
Porter, M. E. (2012). In Guth C. (Ed.), Redefining
german health care moving to a value-based system. Heidelberg; Heidelberg,
Germany ; New York: Heidelberg : Springer.
Preskitt, J. T. (2008). Health care reimbursement:
Clemens to Clinton. Proceedings (Baylor University.Medical
Center), 21(1), 40-44. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2190551/
Rosenbaum, L. (2015). Transitional chaos or enduring
harm? the EHR and the disruption of medicine. N Engl J Med, 373(17),
1585-1588. 10.1056/NEJMp1509961 Retrieved from https://doi-org.ez-proxy.brooklyn.cuny.edu/10.1056/NEJMp1509961
Schimpff, S. (2014). How many patients should A
primary care physician care for? Retrieved from https://medcitynews.com/2014/02/many-patients-primary-care-physician-care/?rf=1
The Robert Graham Center. (2015). Primary care
physician mapper. Retrieved from https://www.graham-center.org/rgc/maps-data-tools/interactive/primary-care-physician.html
United States Government, Accountability Office.
(2014). Electronic health record programs : Participation has
increased, but action needed to achieve goals, including improved quality of
care : Report to congressional committees Washington, District of
Columbia : United States Government Accountability Office.
US Census Bureau. (2016). Quick facts, queens county
(queens borough), new york; united states. Retrieved
from https://www.census.gov/quickfacts/fact/table/queenscountyqueensboroughnewyork,US/PST045216
[1]
Accounting for physicians of general internal medicine, family medicine,
general practice, and pediatrics using data from 2013.
[2]
Recommended patient loads for quality care are 800 patients or less (Schimpff,
2014)
[3]
Assuming patients present at least one symptom and do not suffer from
comorbidity.
[4]
The exception being core assessment number 10, which tests for effective
communication of patient data rather than focusing on patient health.
[5]
Refer to Appendix 1 under the supporting documents.
[6]
Refer to Appendix 2 under the supporting documents.



No comments:
Post a Comment